This year’s CPHI seminar series is titled “From Innovation to Dissemination”. The series builds upon the University of Pennsylvania’s annual theme for 2015/16 – The Year of Discovery that focuses on both the long-range, planned and calculated research toward an intended goal as well as the more “spontaneous and serendipitous” discoveries.
This year’s series will create a forum for cross-sector communication around innovative public health solutions. Seminars will present real world solutions to complex problems including new finance mechanisms to fund public health initiatives, the use of digital health technology, and innovative approaches to address the opioid epidemic.
Throughout each series, we aim to encourage different perspectives to add to the conversation; we hope to foster current collaborations and spark new ones; and we hope to instill the importance of always searching for new ways to improve health.
Save-the-date! Fall Semester Seminar Line-up
Seminar Kickoff Event: Voices of Health Exhibit and CPHI Overview
September 9th (Wednesday) 4:30pm – 6:00pm | Register
Claudia Cohen Hall – Terrace Room
Come and join CPHI Fellows and the public health community to learn about CPHI and the resources that we have to offer. Wine reception to follow as you stroll through a photo exhibit that documents what the domain of “health” means to the Penn community. We asked over 300 students, staff, faculty members and community residents “what words come to mind when you think about health?”. This photo exhibit documents what they said.
Moving an Innovative Idea into Action: It’s Not as Hard as You May Think
Roy Rosin, MBA
Chief Innovation Officer
Penn Medicine’s Center for Innovation
September 18th (Friday) 12:00pm – 1:30pm | Register
Claudia Cohen Hall – Terrace Room
Join us as we hear from Roy Rosin, Chief Innovation Officer from Penn Medicine’s Center for Innovation where he works with thought leaders across the health system to turn ideas into measurable impact in the areas of health outcomes, patient experience and new revenue streams. Roy will talk about practical ways to turn your innovative idea into a reality. Roy received his MBA from the Stanford Graduate School of Business and graduated with honors from Harvard College. Outside of work he serves as a board member and angel investor for venture funded startups, an advisor to Fortune 100 companies and a coach to his son’s little league baseball teams.
Digital Health Innovation
Chris Murphy, PhD
Associate Professor of Practice
Department of Computer and Information Science University of Pennsylvania
Nalaka Gooneratne, MD, MSc
Associate Professor of Medicine UPenn, Presby, & VA
October 5th (Monday) 12:00pm – 1:30pm | Register
Krishna Singh Center for Nanotechnology
Move out of your comfort zone and into the world of Digital Health Technology. Drs. Murphy and Gooneratne will each bring their own expertise and demonstrate how to leverage digital technology into practical applications to improve health outcomes. Dr. Murphy is an Associate Professor of Practice in the Department of Computer & Information Science at the University of Pennsylvania, and Director of the Masters of Computer & Information Technology program. Dr. Gooneratne is a physician specializing in sleep disorders. In addition to his research (funded by NIA, NCCAM and NHLBI), he is the Associate Program Director for the Clinical and Translational Research Center, and the mHealth service (mobile app development) within the Institute for Translational Medicine and Therapeutics (ITMAT). He is also the director of the Masters in Translational Research Entrepreneurial Science track.
A New Approach to Address Social Challenges: Impact Bonds
Jeff Liebman, PhD
Professor of Public Policy
Harvard Kennedy School of Government
Moderated by:
Ezekiel Emanuel, PhD
Vice Provost for Global Initiatives
Chair of the Department of Medical Ethics and Health Policy
The University of Pennsylvania
October: Exact Date TBD
Social Impact Bonds (SIBs), often referred to as Pay-For-Success, are a novel funding approach that combine components of results- or performance-based financing and public-private partnerships, which have been used to fund public services for many decades. With a SIB, financing is provided upfront rather than when results are attained and results are related to outcomes as opposed to outputs. To date, 44 SIBs are being utilized in developed countries to, among other social issues, provide high-quality preschool education, reduce prison recidivism, avoid foster care placement, and increase youth employment.
Dr. Liebman will walk us through the SIB model and see how we can apply it to fund public health services. Dr. Liebman, Malcolm Wiener Professor of Public Policy, studies tax and budget policy, social insurance, poverty, and income inequality. During the first two years of the Obama Administration, Liebman worked at OMB, first as Executive Associate Director and Chief Economist and then as Acting Deputy Director. From 1998 to 1999, Liebman served as Special Assistant to the President for economic policy and coordinated the Clinton Administration’s Social Security reform technical working group.
Advocacy & Influence: Innovations Addressing Homelessness
Sister Mary Scullion
President & Executive Director
Project HOME
December 8th (Tuesday) 12:00pm-1:30pm| Register
Class of ’49 Auditorium
Sister Mary Scullion, R.S.M. is a Philadelphia-based American Roman Catholic Religious Sister and activist, named by “Time” as one of the “100 Most Influential People in the World” in 2009, alongside Michelle Obama and Oprah Winfrey. Scullion has been involved in service work and advocacy for homeless and mentally ill persons since 1978. In 1989, she co-founded Project H.O.M.E., a nationally recognized organization that provides supportive housing, employment, education and health care to enable chronically homeless and low-income persons to break the cycle of homelessness and poverty in Philadelphia. Join us to hear Sister Mary’s powerful voice on political issues affecting homelessness and mentally ill persons. She will address how advocacy efforts can result in long-term sustainable policy and law changes.
Behavioral Economics: How People Process Information and Make Decisions
Kevin Volpp, MD, PhD
Director
Center for Health Incentives and Behavioral Economics, Leonard David Institute
January 12th (Tuesday) 12:00pm-1:30pm| Register
Arch 208 Auditorium, 3601 Locust Walk
Dr. Volpp is the founding Director of the Center for Health Incentives and Behavioral Economics at the Leonard Davis Institute of Health Economics (LDI CHIBE), Director of the NIH-funded Penn CMU Roybal P30 Center in Behavioral Economics and Health, Vice Chairman for Health Policy for the Department of Medical Ethics and Policy, and a Professor of Medicine at the Perelman School of Medicine at the University of Pennsylvania and Health Care Management at the Wharton School. He is a core faculty member of the Center for Health Equity Research and Promotion (CHERP) and a board certified practicing physician at the Philadelphia VA Medical Center.
The Science of Simple, Low-Cost Health and Safety Interventions
Charles Branas, PhD
Professor of Epidemiology
University of Pennsylvania
Sara Heller, PhD
Associate Professor of Criminology
University of Pennsylvania
February 25th (Thursday) 12:00pm-1:30pm| Register
Location TBD
Dr. Branas works to improve health and healthcare and is recognized for his efforts to reduce violence and enhance emergency care. Much of his work incorporates human geography and place-based change. His studies have taken him to cities and small towns across the US and other countries. Dr. Branas has served on boards and offered scientific expertise for numerous groups including the NIH, the CDC, and the National Academies in the US, as well as national scientific organizations in Canada, South Africa, New Zealand, and the Netherlands. His work has been cited by the US Supreme Court and Congress. He is a past President of the Society for Advancement of Violence and Injury Research, an elected member of the American Epidemiological Society, and affiliated faculty at the University of San Carlos in Guatemala.
Professor Heller focuses primarily on field experiments testing the effects of treatment interventions on crime, education, and other life outcomes. She is investigating the effects of cognitive behavioral therapy-based programming on juvenile crime and schooling outcomes. She is also conducting two related studies on the effects of summer jobs on youth, especially on their crime and labor market outcomes.
Innovative Practices to Address the Opioid Epidemic
Matthew Hurford, MD
Vice President of Medical Affairs
Community Care Behavioral Health Community
March 18th (Friday) 12:00pm-1:30pm| Register
Location TBD
Dr. Hurford is Vice President of Medical Affairs for Community Care Behavioral Health Organization one of the country’s largest not-for-profit behavioral health managed care organization. Headquartered in Pittsburgh, Community Care serves over 750,000 Medicaid beneficiaries across Pennsylvania by facilitating the ongoing evolution of the behavioral health system toward one that embraces the journey of healing, transformation, and empowerment.
As VP of Medical Affairs at Community Care, Dr. Hurford provides leadership in the development of new business opportunities and program development including physical health/behavioral health integration and innovative healthcare payment models.
Prior to joining Community Care, Dr. Hurford served as the Chief Medical Officer of the City of Philadelphia’s Department of Behavioral Health and Intellectual Disability Services (DBHIDS) and Community Behavioral Health (CBH), a not-for-profit behavioral health managed care organization.
Additional training and educational opportunities:
LGBT Transgender Symposium: Training for Healthcare Providers
December 10th, 8:30am-1:00pm
Biomedical Research Building
Qualitative Research Institute
January 7th – 9th (all day training)
More details coming soon!
For questions about our seminar series, please contact Elizabeth Devietti eldevi@mail.med.upenn.edu
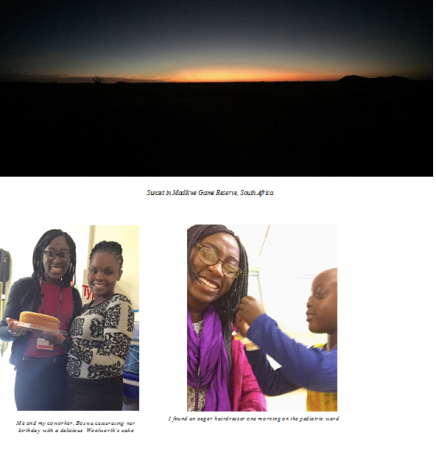 isn’t a “best places to see” blog post. I began my summer in Sunyani, Ghana, visiting my family for what was one of our largest gatherings to date. I packed for Ghana as I’ve always packed for Ghana; even in “winter” Ghana is a balmy 80 ºF. In late May, I said goodbye to my family who stood puzzled as I boarded a flight to Botswana. They were confused by my decision to conduct research in Botswana rather in Ghana. “Go with God,” my grandfather said, “and remember to bring the results back home.”
isn’t a “best places to see” blog post. I began my summer in Sunyani, Ghana, visiting my family for what was one of our largest gatherings to date. I packed for Ghana as I’ve always packed for Ghana; even in “winter” Ghana is a balmy 80 ºF. In late May, I said goodbye to my family who stood puzzled as I boarded a flight to Botswana. They were confused by my decision to conduct research in Botswana rather in Ghana. “Go with God,” my grandfather said, “and remember to bring the results back home.”







 Women’s Focus Group
Women’s Focus Group